Globally, anemia is highly prevalent among women of reproductive age. At least 20 million women worldwide have severe anemia. As maternal blood hemoglobin level decreases, the risk of maternal and infant death during pregnancy increases. A new study recently published in the journal, “Lancet”, reported that moderate-to-severe prebirth anemia among women increases the risk of postpartum hemorrhage. The study also confirmed the dose-response relationship between prebirth hemoglobin and postpartum hemorrhage. Besides, women with severe anemia were at an increased risk of death or near miss due to hemorrhage compared to those with moderate anemia.
This prospective cohort study collected data from the WOMAN-2 [World Maternal Antifibrinolytic-2]) trial, an ongoing, randomized, placebo-controlled trial, involving women from low-income and middle-income countries. Women with moderate-to-severe anemia (hemoglobin concentration <100 g/L or packed cell volume <30%) and vaginal delivery (n = 10,620 [10,561 women had complete outcome data]; mean age = 27.1 years) were enrolled in the study. Prebirth hemoglobin was measured after arrival at the hospital and just before giving birth while postpartum hemoglobin was measured within 24 h of birth. Postpartum hemorrhage was defined as (I) clinical postpartum hemorrhage (estimated blood loss of at least 500 mL or any blood loss sufficient to compromise hemodynamic stability within 24 h of birth); (II) WHO-defined postpartum hemorrhage (estimated blood loss of 500 mL or more from the genital tract within 24 h of a vaginal birth); and (III) calculated postpartum hemorrhage (calculated estimated blood loss of 1000 mL or more). Multivariable logistic regression analysis was used to examine the association between hemoglobin levels and postpartum hemorrhage (confounding factors were adjusted).
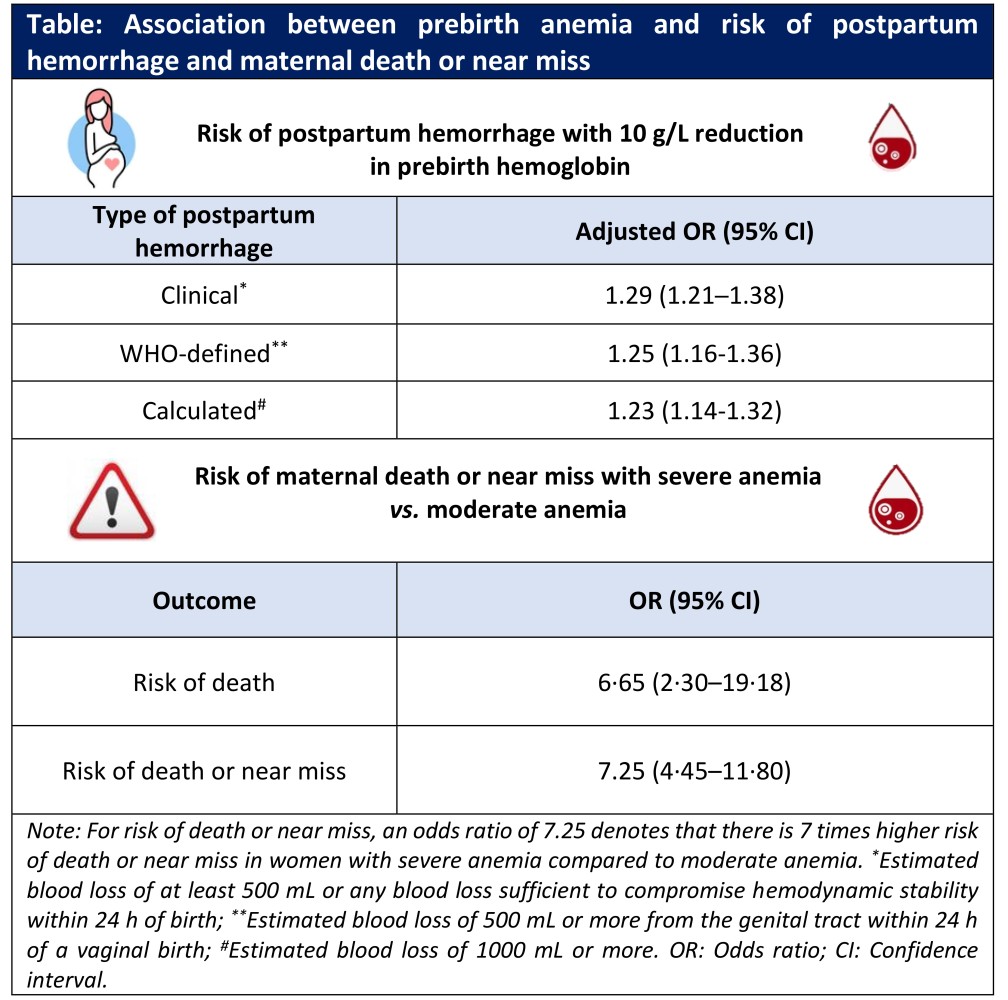
Key results of the study are summarized below:
- Moderate anemia was reported in 83.2% (n = 8,791) whereas severe anemia was reported in 16.8% (n = 1,770) of the recruited women. Mean prebirth hemoglobin was 80·7 g/L.
- Women with severe anemia had 7-times higher risk of death or near misscompared to those with moderate anemia.
- Clinical postpartum hemorrhage was reported in 742 women, with higher occurrence in women with severe anemia (11.2%) than in those with moderate anemia (6.2%).
- Severe anemia was associated with significantly higher mean estimated blood loss compared to moderate anemia (340 mL vs. 301 mL; p<0.0001).
- A 10 g/L reduction in hemoglobin at prebirth was associated with increased risk of clinical, WHO-defined, and calculated postpartum hemorrhage (Table).
Clinical implications
- This study highlights that anemia in women is a strong risk factor for postpartum hemorrhage and associated death.
- Prevention and treatment of anemia in women of reproductive age is urgently recommended for reducing maternal and infant mortality at the time of delivery.
(Source: WOMAN-2 trial collaborators. Maternal anaemia and the risk of postpartum haemorrhage: A cohort analysis of data from the WOMAN-2 trial. Lancet Glob Health. 2023;S2214-109X(23)00245-0. Doi:10.1016/S2214-109X(23)00245-0)