A survey by Hill et al., published in the “Journal of the American Heart Association”, found that individuals with a recent history of clinically significant weight loss (CSWL) showed greater adherence to American Heart Association’s Life’s Essential 8 (LE8) recommendations for ideal cardiovascular (CV) health. Individuals who had achieved CSWL over the past year had better overall diet quality, greater levels of physical activity, and greater implementation of evidence-based weight loss strategies as against individuals with weight loss <5%, weight maintenance, or weight gain.
This retrospective, cross-sectional study analyzed data about weight loss history and behaviors related to CV risk among US adults (n = 20,305; mean age: 47.3 ± 0.3 years; 50.4% men) in the 2007–2016 National Health and Nutrition Examination Survey (NHANES) cycles. Adherence to LE8 recommendations (which includes recommendations for body weight, blood pressure, cholesterol, blood sugar, smoking, physical activity, diet, and sleep), diet quality (Healthy Eating Index), and weight loss strategies were compared between adults with intentional CSWL ≥5% (n = 2,840) and non-CSWL <5%, weight maintenance, or weight gain (n = 17,465) over the past one year. Data were obtained using standardized questionnaires, physical health examinations, and 24-hour dietary recalls. Analysis of covariance (ANCOVA) was performed to evaluate the mean differences and standard errors for the LE8 scores between individuals with and without CSWL, controlling for age, sex, race or ethnicity, and poverty-income ratio.
The study results are summarized below:
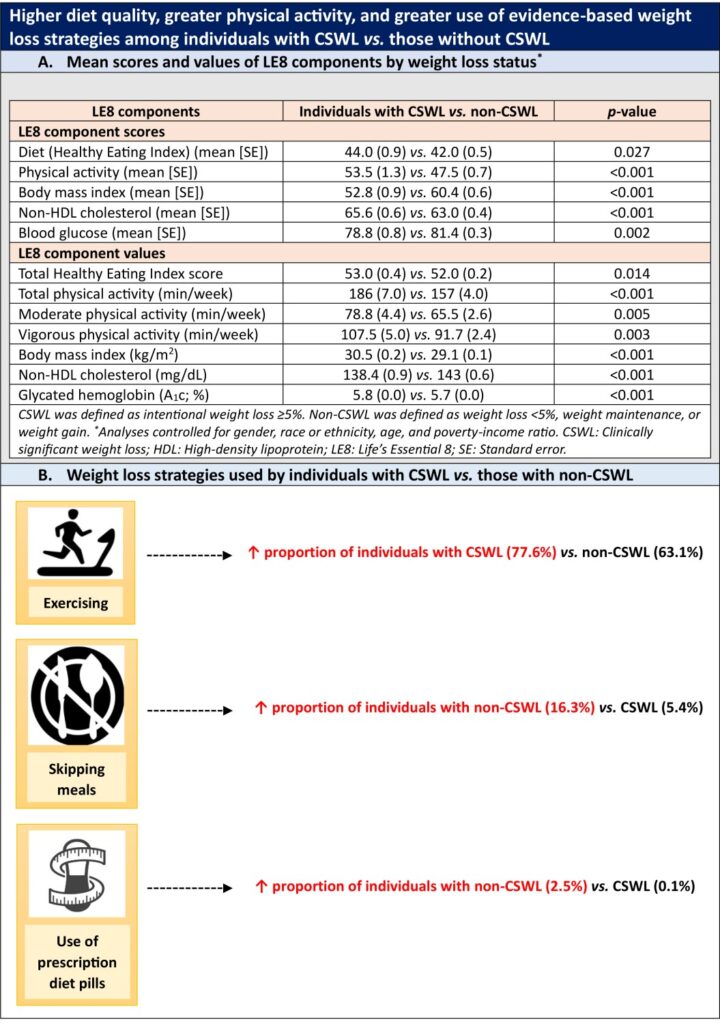
- Individuals with CSWL had significantly higher mean body mass index and A1c and lower non–high-density lipoprotein cholesterol relative to those without CSWL (Graphic A). They also reported better diet quality as well as greater levels of moderate and vigorous physical activity, translating to higher LE8 metric scores for diet and physical activity (Graphic A).
- The mean LE8 composite CV health score between individuals with and without CSWL was similar (63.4 vs. 63.0; p= 0.313).
- With regard to dietary components, individuals with CSWL had significantly better diet quality for total protein foods (p = 0.026), refined grains (p <0.001), and added sugars (p <0.001) but poorer diet quality for sodium (p<0.001).
- A higher proportion of individuals in the CSWL group reported following an exercise regimen to achieve weight loss as against those in the non-CSWL group (p = 0.016; Graphic B).
- Notably, a greater proportion of individuals without CSWL skipped meals (p = 0.002) and used prescription diet pills (p <0.001) (Graphic B).
Clinical implications
- Implementation of core modifiable health behaviors as recommended by the American Heart Association’s LE8 is a cornerstone for alleviating CV risk and promoting safe weight management strategies for adults.
- Improvements in all health parameters may not be evident immediately after weight loss achieved through behavioral change for improved CV health. Hence, individuals with a recent history of CSWL should be encouraged to sustain weight loss so as to derive long-term CV health benefits.
- This study sheds light on the potential relationships between diet quality, weight loss strategies, and CV health among individuals attempting to lose weight. Improved understanding of current practices for weight loss, especially relating to the LE8 recommendations, may help to develop pragmatic interventions and public health policies for disease prevention and weight management approaches in the future.
(Source: Hill EB, Cubellis LT, Wexler RK, Taylor CA, Spees CK. Differences in adherence to American Heart Association’s Life’s Essential 8, diet quality, and weight loss strategies between those with and without recent clinically significant weight loss in a nationally representative sample of US adults. J Am Heart Assoc. 2023;12(8):e026777. Doi: 10.1161/JAHA.122.026777)