
Sodium intake is vital for maintaining several physiological functions in the body, including fluid balance, cellular homeostasis, and nutrient absorption. The link between salt intake and hypertension is well documented, but the association between high salt intake and type 2 diabetes (T2D) remains underexplored due to challenges associated with determining dietary sodium intake.
Numerous studies have demonstrated that the frequency of adding salt to foods, typically at the table, serves as an effective indicator of discretionary sodium intake as well as reflects an individual’s long-term preference for salt taste and sodium consumption. A recent study by Wang et al., published in the journal, Mayo Clinic Proceedings, reported the association between increased frequency of adding salt to foods and heightened risk of T2D, majorly influenced by body mass index and inflammation.
The study analyzed the data of 4,02,982 participants (aged 37 to 73 years) from the UK Biobank, a prospective population-based study and assessed the associations between the frequency of adding salt to food, other than cooking, and the risk of T2D. At baseline, the participants were free from diabetes, chronic kidney disease, cancer, or cardiovascular disease. Data on frequency of salt addition was collected through a touch-screen questionnaire. Salt usage, other than used in cooking, was categorized as – never/rarely, sometimes, usually, always, and prefer not to answer. Details on diabetes occurrence was obtained through medical history, data from hospital admissions, questionnaires, or death register. Urinary biomarkers such as spot urinary sodium, ratio of sodium and potassium, and estimated 24-hour urinary sodium excretion were assessed and their relationship with the risk of diabetes was analyzed. The mean follow-up period was 11.9 years.
The study results are summarized below:
1) Salt intake and 24-hour urinary excretion: At baseline, higher frequency of self-reported salt intake was associated with greater urinary sodium excretion (p <0.001).
Ø “Never/rarely” group: 3.19 g
Ø “Sometimes” group: 3.23 g
Ø “Usually” group: 3.27 g
Ø “Always” group: 3.30 g
2) Incidence of diabetes: At follow-up, a total of 13,120 participants were reported to have diabetes.
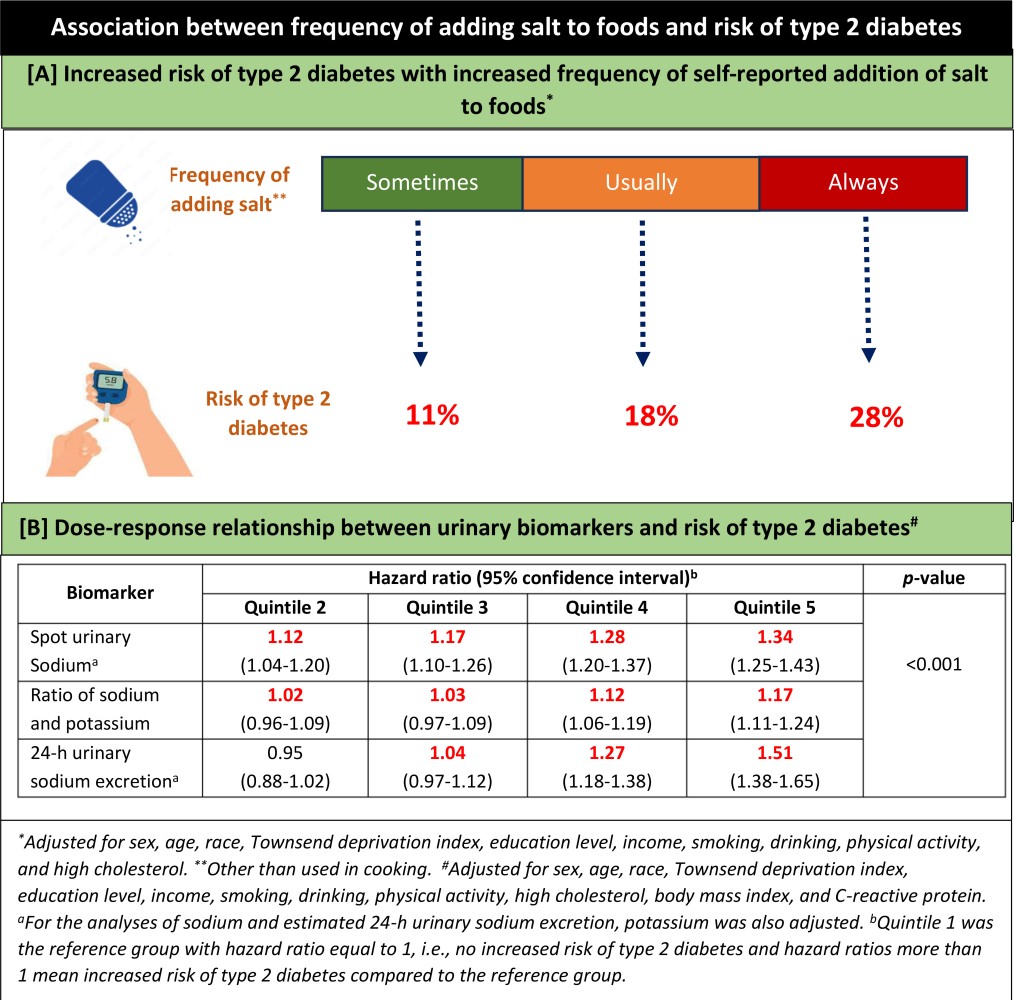
3) Frequency of adding salt to foods and risk of diabetes: Significantly higher risk for development of T2D was reported with higher self-reported addition of salt to foods across the salt usage groups, compared to individuals who never/rarely added salt to their food (p <0.001; Graphic [A]).
4) Urinary biomarkers and risk of diabetes: Higher values of urinary biomarkers, viz., spot urinary sodium, ratio of sodium and potassium, and estimated 24-hour urinary sodium excretion were associated with an increased risk of T2D among the participants (p <0.001; Graphic [B]).
5) Potential mediators (adiposity measures and inflammation) and risk of diabetes: The association between adding salt to foods and the risk of T2D was influenced and significantly mediated by body mass index (33.8%), waist-to-hip ratio (39.9%), and C-reactive protein (8.6%) (Note: percentages are mediation effects).
Clinical implications
1) The study results support actionable measures to promote reducing the frequency of adding salt during meals. This can be a crucial strategy in preventing development and progression of T2D, especially in high-risk populations.
2) The potential use of spot urinary sodium as a future biomarker for assessing the risk of T2D can enhance the precision of risk evaluation for T2D, allowing the healthcare practitioners to adopt more proactive and targeted approaches in disease prevention and management.
(Source: Wang X, Ma H, Kou M, Tang R, Xue Q, Li X, Harlan TS, Heianza Y, Qi L. Dietary sodium intake and risk of incident type 2 diabetes. Mayo Clin Proc. 2023:S0025-6196(23)00118-0. Doi: 10.1016/j.mayocp.2023.02.029)
