
Insufficient sleep is linked to elevated risk for type 2 diabetes among general population. However, the impact of chronic insufficient sleep on glucose metabolism in women remains uncertain. A recent study by Zuraikat et al., published in the journal, Diabetes Care that even mild sleep restriction (90 minutes per night) over an extended period may result in elevated fasting insulin levels and increased insulin resistance in women. The increase in insulin resistance was higher among postmenopausal women compared to premenopausal women. Moreover, changes in body fat, a known risk factor for insulin resistance, did not mediate the negative impact of reduced sleep on glucose metabolism [1].
This randomized, crossover study enrolled 38 women without cardiometabolic diseases (age range: 20–75 years; post-menopausal women, n = 11; total sleep duration by actigraphy: 7–9 hour/night). The study participants underwent two 6-week phases in random order, with a washout period of 4–6 weeks:
1. Adequate sleep (AS) group: They received adequate sleep of >7 hours/night.
2. Sleep restriction (SR) group: The bedtime was delayed by 1.5 hour/night; i.e., they had 1.5.h of less sleep/night.
Outcomes included fasting plasma glucose and insulin levels, as well as insulin resistance (using the Homeostatic Model Assessment for Insulin Resistance; HOMA-IR). Compliance with sleep schedules was assessed using wearable devices. Along with insulin and glucose levels, body fat was also determined throughout the study [1,2].
The study results are summarized below [1]:
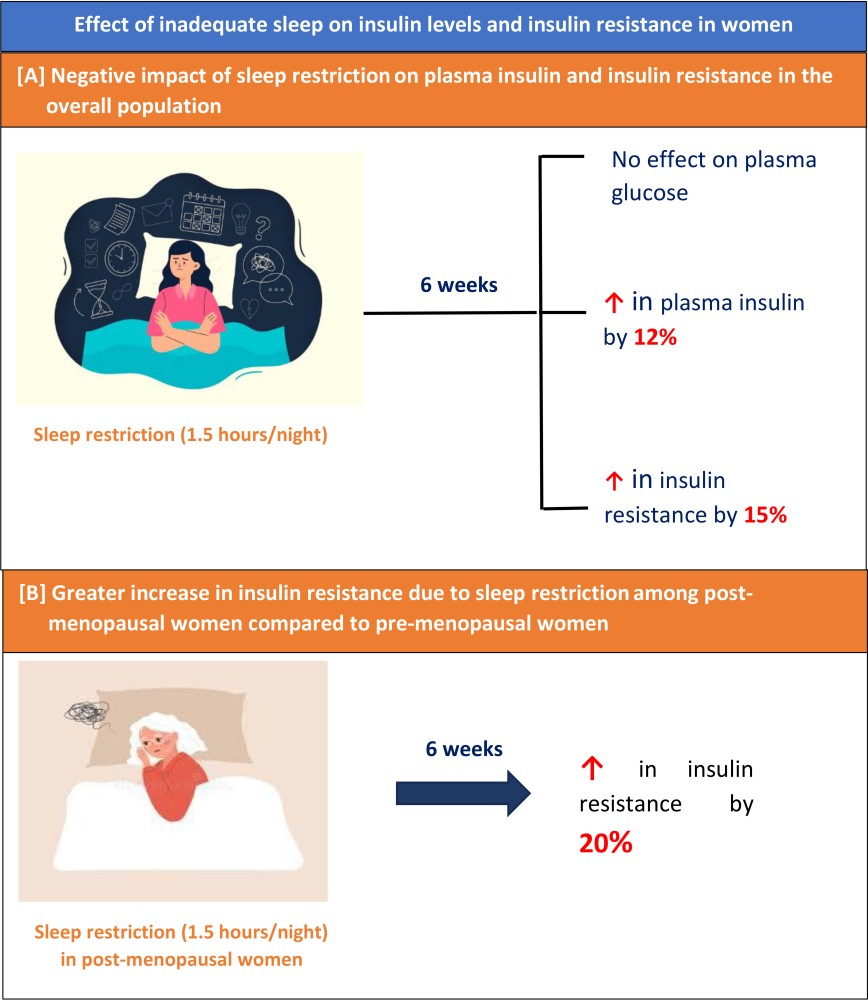
- Although sleep inadequacy appeared to have no effect on plasma glucose levels, sleep restriction for even 90 minutes/night for 6 weeks resulted in significant increase in the fasting insulin levels as well as insulin resistance compared to participants with adequate sleep (β = 6.8 ± 2.8 pmol/L and β = 0.30 ± 0.12; p = 0.016) (Graphic A).
- Lack of sleep appeared to have a greater impact on insulin resistance among postmenopausal women compared to premenopausal women. (β = 0.45 ± 0.25 vs. β = 0.27 ± 0.13; p = 0.042) (Graphic B).
- Changes in body fat did not mediate the impact of sleep duration on insulin resistance.
Clinical implication [1,2]: This study confirmed that adequate sleep duration is a potentially modifiable risk factor in the prevention of insulin resistance in women, especially after menopause. Addressing sleep patterns could be an important component of diabetes prevention strategies for the improvement of overall metabolic health of women.
(References: 1. Zuraikat FM, Laferrère B, Cheng B, et al. Chronic insufficient sleep in women impairs insulin sensitivity independent of adiposity changes: Results of a randomized trial. Diabetes Care. 2023;dc231156. Doi:10.2337/dc23-1156 2. Columbia University Irving Medical Center. Shortening sleep time increases diabetes risk in women. ScienceDaily [Internet]. 2023 [cited 2023 Nov 29]. Available from: https://www.sciencedaily.com/releases/2023/11/231113111633.htm)
