
Childhood obesity is a growing global health issue, with an estimated 40 million children under the age of 5 years classified as overweight or obese in 2020. The most rapid increases are occurring in Asia, the Middle East, and Latin America. The South Asian individuals (originating from the Indian subcontinent) exhibit a unique risk profile of higher prevalence of central adiposity and increased cardiometabolic risk predisposes them to diabetes and cardiovascular disease (CVD) in adulthood. South Asian newborns and children have lower birth weight and higher body fat relative to the body size compared to their western counterparts. This “thin-fat” phenotype persists for several generations and is associated with long-term metabolic and cardiovascular complications.
Body mass index (BMI), although widely used, can underestimate fat distribution in South Asian individuals. Alternative measures such as skinfold thickness may provide more accurate assessments of adiposity in this group. While numerous studies link prenatal and perinatal factors (e.g., maternal nutrition, gestational diabetes, and early-life feeding patterns) to childhood obesity, most research has focused on the White European populations. Additionally, obesity is often assessed at a single time point rather than longitudinally, missing the dynamic nature of early growth. There is a critical need for more ethnically inclusive, longitudinal studies to better understand adiposity trajectories in South Asian children and undertake targeted early interventions.
A study by Azab SM et al., published in the journal “JAMA Network Open”, investigated how prenatal and early childhood factors influence adiposity trajectories in South Asian children, focusing on the role of modifiable lifestyle factors, based on the data from the START cohort (n = 903), which was validated using data from the FAMILY and BiB cohorts. Adiposity was measured by area under the curve (AUC) for skinfold thickness from birth to age 3 years. Six modifiable factors—maternal skinfolds, gestational weight gain, diet, breastfeeding, physical activity, and screen time—were significantly associated with AUC. Breastfeeding (β = −1.68) and physical activity (β = −0.33) were protective, while screen time (β = 0.49) increased the risk for obesity. A cumulative risk score showed a graded association with adiposity. The findings support early interventions to reduce childhood adiposity (See Graphic).
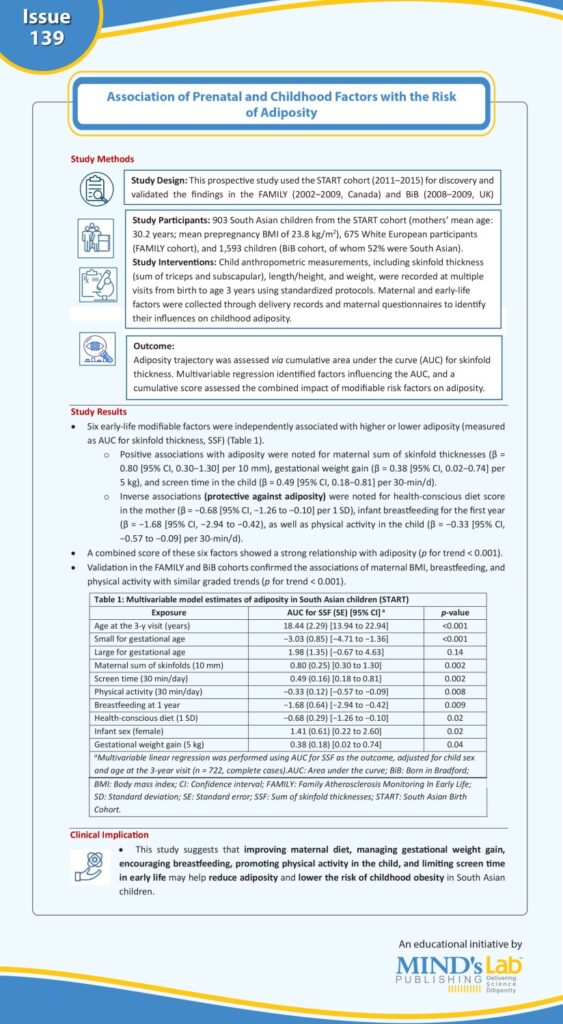
(Source: Azab SM, Naqvi S, Rafiq T, Beyene J, Deng W, Lamri A, Morrison KM, Teo K, Santorelli G, Wright J, Williams NC, de Souza RJ, Wahi G, Anand SS. Trajectory of early life adiposity among South Asian children. JAMA Network Open. 2025;8(4):e254439. Doi:10.1001/jamanetworkopen.2025.4439)
