A recent study published in JAMA Otolaryngology-Head & Neck Surgery highlights the efficacy of olfactory training in restoration of lost sense of smell due to COVID-19-associated post-viral olfactory dysfunction (PVOD). Smelling essential oils stimulates healing and regrowth of the nerves necessary for message transmission to the brain. A greater improvement in smelling power was observed when the scents were chosen by the patients. Furthermore, showing digital pictures of the smelled oils resulted in even better clinical outcome.
A randomized, single-blinded trial included 275 patients (aged 18 to 71 years) with current loss of smell (for 3 months or longer) due to COVID-19 infection, initially diagnosed within 2 weeks of infection, in order to determine and compare the efficacy of olfactory training with or without using visual images of the scents and to evaluate the effect of patient-preferred odors and physician-assigned odors on the outcome.
Patients were divided into 4 study groups (n = 240) and 1 control group (n = 35). Patients in the study groups sniffed 4 essential oils (either physician-assigned [rose, lemon, eucalyptus, and clove] or patient-preferred [lemon, vanilla, sandalwood, lavender, and eucalyptus]) for 15 seconds with a 30-second rest in between odors, with (bimodal) or without (unimodal) visual training, i.e., using images of the scents. The patients in the control group did not receive olfactory training or any other treatment for 3 months. Post-training olfactory assessment were completed using the University of Pennsylvania Smell Identification test (UPSIT) and Clinical Global Impressions (CGI) Severity and Improvement scores. The results are summarized below (per-protocol analysis):
- More patients in the study groups (37.6%) showed improvement in olfactory loss compared to the control group (24%).
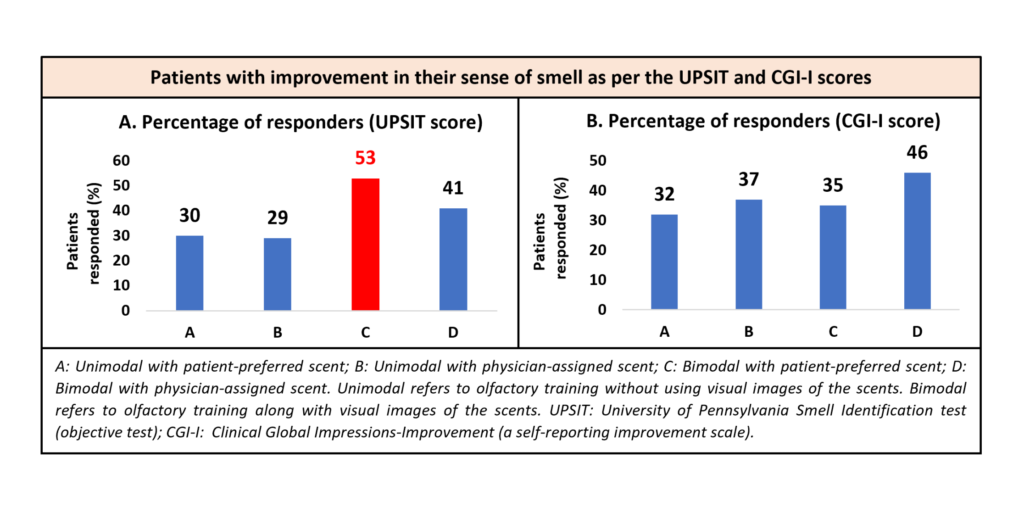
- Within the study groups, a greater number of patients responded (characterized by a 4-point change or greater on the UPSIT score) to bimodal training with patient-preferred scents (see Graph A).
- Greater number of patients self-reported clinically significant improvement in the smelling power after olfactory training (35%) compared to the control group (17%) as per the CGI-I scores. (see Graph B).
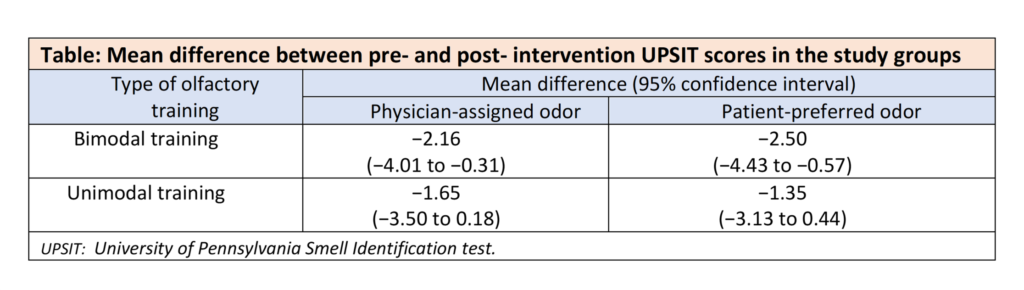
- Change in the UPSIT scores was similar after the training in the study groups (see the Table below).
Clinical implication:
- Individuals with olfactory loss post-COVID-19 infection may benefit from olfactory training using essential oils.
- Usage of patient-preferred scents (lemon, vanilla, sandalwood, lavender, and eucalyptus) in olfactory training may increase the patient’s adherence to the intervention, resulting in better clinical outcome, compared to the physician-assigned classic odors.
- Modification in olfactory training by adding visual stimulation can improve olfactory outcomes by potentiating olfactory neuroplasticity.
- Olfactory training is a low-cost, non-invasive and minimal-risk intervention that can be recommended to patients with PVOD, as it may provide additional benefits in olfaction restoration.
(Reference: Efficacy of combined visual-olfactory training with patient-preferred scents as treatment for patients with COVID-19 resultant olfactory loss: A randomized clinical trial. JAMA Otolaryngol Head Neck Surg. 2022;10.1001/jamaoto.2022.4112. Doi:10.1001/jamaoto.2022.4112)
